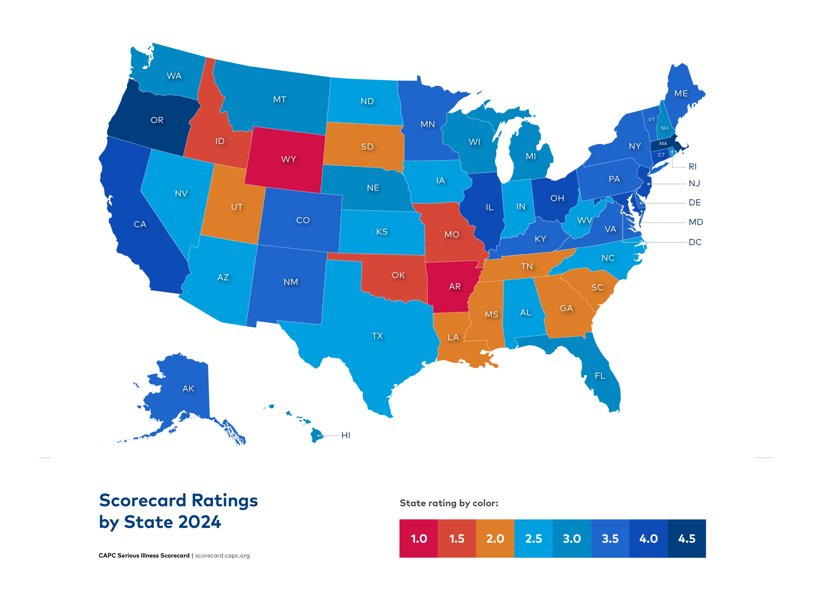
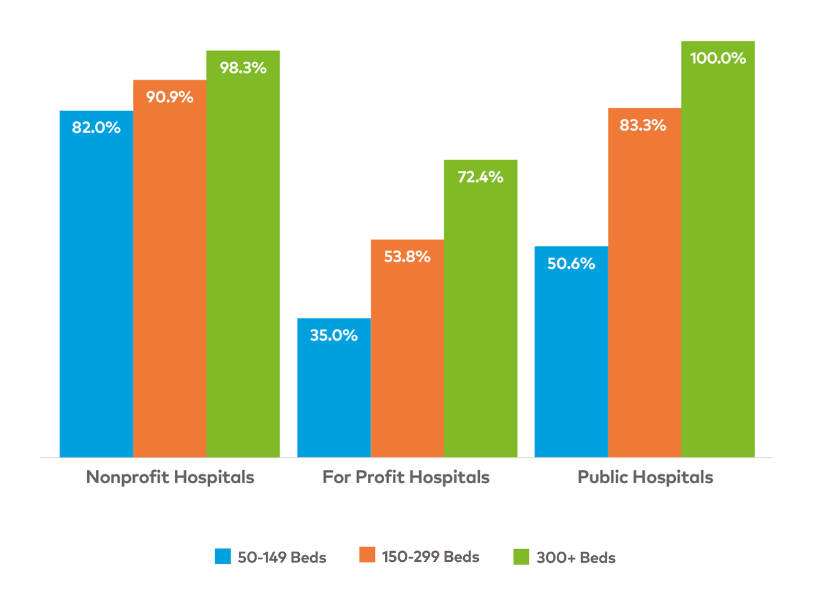
Action at the federal and state levels is needed to expand palliative care access to all people living with serious illness, and their families and caregivers
At the federal level, the Palliative Care and Hospice Education and Training Act (PCHETA, S. 2243 in the 118th Congress) remains an essential vehicle to grow the specialty palliative care workforce and increase the capacity of all non-palliative care clinicians in communication and pain and symptom management; expand palliative care research; and increase palliative care awareness among the general public. Visit the Patient Quality of Life Coalition’s (PQLC) Advocacy page for more information.
At the state level, CAPC encourages state policymakers and champions to explore opportunities for action in the following domains:
WORKFORCE
Expand the specialty palliative care workforce pipeline to meet the needs of patients living with a serious illness. Recommendations include (but are not limited to):
- Establish or expand loan forgiveness programs for certified clinicians who work as palliative care specialists in your state.
- Provide grants and other supports to enable palliative care teams to provide remote consultations to rural hospitals and federally qualified health centers, addressing key disparities in access to palliative care.
Payment
Improve financing and financial incentives to ensure equitable and reliable access to palliative care. Recommendations include (but are not limited to):
- Incorporate essential components of palliative care into relevant Medicaid programs (such as Health Homes, Managed Long-term Care Plans, or Home and Community Based Services). This can include revising enrollee assessments to include functional impairment, symptom distress, and caregiver burden, or inserting communication training requirements for care managers and other clinicians.
- Create a process to involve multiple interested parties, in conjunction with the state department of health, to inform the development of Medicaid reimbursement and quality control measures for interdisciplinary, community-based palliative care.
- Expand Department of Insurance regulations to require all state health plans to cover encounters by a palliative care specialist, without visit maximums or other impediments.
Quality / Standards
Expand accountability for access to high-quality care delivery. Recommendations include (but are not limited to):
- Use state policies and regulations to define palliative care services and standards.
- Add a palliative care module to the state Behavioral Risk Factor Surveillance System (BRFSS) questionnaire to better understand palliative care delivery from the consumer perspective.
Clinical Skill-Building
Expand all clinician training in communication; pain and symptom management; caregiver assessment and support; and care over time and settings. Recommendations include (but are not limited to):
- Revise state health professional licensure and continuing education requirements to include a minimum number of hours of instruction in both pain/symptom management skills and serious illness communication skills, with particular attention to best practices in equitable care. There are now five states requiring implicit bias training for their physicians, and others may follow.
Public and Clinician Awareness
Improve knowledge about palliative care and its benefits. Recommendations include (but are not limited to):
- Create a state-level awareness campaign to educate the public and providers on what palliative care is and who can benefit.
Palliative care leaders in a given state may have more targeted recommendations to improve access and quality, and should be consulted before embarking on any new initiative. Visit CAPC’s State Policy Toolkit and the National Academy for State Health Policy (NASHP) Palliative Care Resource Center for more information.